Adenomyosis is a condition in which tissue that normally lines the uterus (endometrium) also grows within the muscular walls of the uterus. This is most likely to happen late in your childbearing years and after you’ve had children.
Adenomyosis isn’t the same as endometriosis – a condition in which the uterine lining becomes implanted outside the uterus – although women with adenomyosis often also have endometriosis. The cause of adenomyosis remains unknown, but the disease typically disappears after menopause. For women who experience severe discomfort from adenomyosis, there are treatments that can help, but hysterectomy is the only cure.
Although adenomyosis can be quite painful, the condition is generally harmless. Learn more about adenomyosis, including its signs and symptoms, when you should see a doctor and what the best treatment might be for you.
The Fibroid Treatment Collaborative is dedicated to the comprehensive multi-disciplinary approach to the management of pelvic pain, abnormal bleeding and adenomyosis. Located in Chicago, Illinois and Austin, Texas, we are minimally invasive gynecologic surgeons, radiologists, pain specialists, reproductive endocrinologists and physical therapists working in collaboration to plan your treatment. We offer a personal treatment plan that takes into account the patient’s personal preferences.
Symptoms of Adenomyosis
In some women, adenomyosis is “silent” – causing no signs or symptoms – or only mildly uncomfortable. But other women with adenomyosis may experience:
- Heavy or prolonged menstrual bleeding
- Severe cramping or sharp, knife-like pelvic pain during menstruation (dysmenorrhea)
- Menstrual cramps that last throughout your period and worsen as you get older
- Pain during intercourse
- Bleeding between periods
- Passing blood clots during your period
Your uterus may increase to double or triple its normal size. Although you might not know if your uterus is enlarged, you may notice that your lower abdomen seems bigger or feels tender.
Tests for Adenomyosis
Your doctor may suspect adenomyosis based on:
- Signs and symptoms
- A pelvic examination, which reveals an enlarged uterus that’s tender to touch
- Ultrasound imaging of the uterus
- Magnetic resonance imaging (MRI) of the uterus
In rare instances, your doctor may take a biopsy of endometrial tissue – a sample of cells from your uterine lining for testing – to verify that your abnormal uterine bleeding isn’t associated with any other serious condition. However, such a biopsy won’t help your doctor confirm a diagnosis of adenomyosis. The only way to establish the diagnosis of adenomyosis is to examine uterine tissue using a microscope after removal of the uterus (hysterectomy).
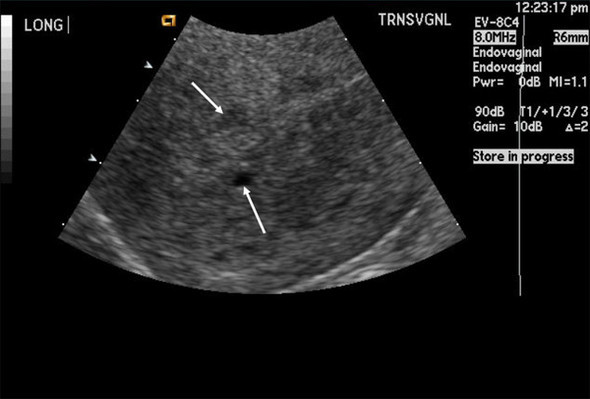

Many women have other uterine diseases that cause signs and symptoms similar to adenomyosis, making adenomyosis more difficult to diagnose. Such conditions include fibroid tumors (leiomyomas), uterine cells growing outside the uterus (endometriosis) and growths in the uterine lining (endometrial polyps). Your doctor may diagnose adenomyosis only after he or she determines there are no other causes for your signs and symptoms.
Although a blood test won’t indicate whether you have adenomyosis, your doctor may suggest testing to assess your menstrual blood loss.
Adenomyosis usually resolves after menopause, so treatment may depend on how close you are to that stage of life.
Treatment of Adenomyosis
Treatment options for adenomyosis include:
- Anti-inflammatory drugs. If you’re nearing menopause, your doctor may have you try anti-inflammatory medications, such as ibuprofen (Advil, Motrin, others), to control the pain. By starting an anti-inflammatory medicine two to three days before your period begins and continuing to take it during your period, you can reduce menstrual blood flow in addition to relieving pain.
- Hormone therapy. Controlling your menstrual cycle through combined estrogen-progestin oral contraceptives, hormone-containing patches or vaginal rings may lessen the heavy bleeding and pain associated with adenomyosis. Progestin-only contraception, such as an intrauterine device containing progestin or a continuous-use birth control pill, often leads to amenorrhea – the absence of your menstrual periods – which may provide relief.
- Presacral Neurectomy. A surgical procedure to interrupt the pain nerve supply, or presacral nerve plexus, to the uterus.
- Hysterectomy. If your pain is severe and menopause is years away, your doctor may suggest surgery to remove your uterus (hysterectomy). Removing your ovaries isn’t necessary to control adenomyosis. Learn more about hysterectomy.
