The Fibroid Treatment Collaborative is dedicated to the comprehensive multi-disciplinary approach to the management of uterine fibroids. The fact is that your situation is unique and deserves an individualized treatment plan. Located in Chicago, Illinois and Austin, Texas, we are minimally invasive gynecologic surgeons, radiologists, pain specialists, reproductive endocrinologists and physical therapists working in collaboration to plan your treatment. We offer a personal treatment plan that takes into account the patient’s personal preferences.
Many issues impact which treatment option a patient may choose. Some of these things include:
- whether or not you are having symptoms from the fibroids
- if you might want to become pregnant in the future
- the size of the fibroids
- the location of the fibroids
- your age and how close to menopause you might be
If you have fibroids but do not have any symptoms, you may not need treatment. This section addresses multiple options for management of uterine fibroids, including:
Close monitoring
Unless fibroids are causing excessive bleeding, significant discomfort or bladder problems, a fibroid treatment is usually not necessary. A woman with fibroids should be evaluated periodically by her health care provider. The visit should include questions about fibroid symptoms and abdominal and pelvic examinations to assess uterine size. Routine pelvic ultrasounds have very little clinical benefit for women without symptoms. Fibroids are likely to increase in size each year until menopause. Changes in fibroid size should not be an indication for a fibroid procedure unless accompanied by disabling symptoms.
Medical Therapy
Currently, the medical treatments available for fibroids can make symptoms better temporarily but they do not make the fibroids go away. For women with heavy bleeding, it is worth trying a medical treatment before undergoing a surgical procedure. Women with pressure symptoms caused by large fibroids will not benefit from any medicines currently available. On the horizon are several promising, new drugs that will treat the fibroids themselves not just the symptoms.
- Oral contraceptive pills and Progestational agents (Provera®, medroxyprogesterone acetate) – Women with heavy menstrual periods and fibroids are often prescribed hormonal medications to try to reduce bleeding and regulate the menstrual cycle. The medications will not cause fibroids to shrink nor will it cause them to grow at a faster rate. If the medication has not improved your bleeding after three months, consult with your doctor. Women over the age of 35 who smoke should not use oral contraceptive pills.
- GnRH agonists (Lupron®) – GnRH agonists are a class of medications that temporarily shrinks fibroids and stops heavy bleeding by blocking production of the female hormone estrogen. Lupron is the most well known of these drugs. Although Lupron can improve fibroid symptoms, it causes unpleasant, menopausal symptoms such as hot flashes and, with long-term use, leads to bone loss. Lupron should be recommended only in very specific circumstances. For example, a woman with very heavy bleeding and profound anemia will likely need a blood transfusion at the time of surgery. However, if she uses lupron for 2-3 months before surgery to make her periods temporarily stop and an iron supplement, the anemia will improve and the need for a blood transfusion will be reduced. In rare instances, a woman with huge fibroids(>10-12 cm) may be encouraged by her doctor to use lupron prior to surgery. Importantly, lupron should not be used solely for the purpose of shrinking fibroids unless surgery is planned because the fibroids will re-grow to their original size and symptoms will return as soon as the lupron is discontinued. Learn more about Lupron.
- GnRH antogonists treat endometriosis and uterine fibroids by blocking the production of hormones that stimulate these conditions. available in oral tablets, these medications have recently transformed medical treatment of fibroids and endometriosis. Learn more about the GnRH antagonists Orilissa, Oriahnn, and Myfembree.
- Intrauterine Devices (IUD) – Although IUD’s are typically used to prevent pregnancy, they have non-contraceptive benefits as well. An IUD that releases a small amount of hormone into the uterine cavity has been shown to decrease bleeding related to uterine fibroids. An IUD can be inserted during a routine office appointment. Ask you doctor for more information about this option. Learn more about the Mirena IUD.
- Lysteda – A new drug, Lysteda, was recently approved by the FDA for the treatment of heavy menstrual bleeding. LYSTEDA is a non-hormonal medication you only take during your period, as opposed to every day. LYSTEDA cannot be used as birth control and because it does not contain hormones, it doesn’t have hormonal side effects. LYSTEDA is FDA-approved to help reduce Heavy Monthly Bleeding (HMB). LYSTEDA was also shown to help make a meaningful difference as early as the first menstrual cycle and for all cycles studied. Learn more about Lysteda.
Radiofrequency Ablation of Uterine Leiomyoma
Acessa – The Acessa procedure is a new minimally-invasive, same-day (outpatient) therapy for fibroids. It uses a technology called radiofrequency ablation. At laparoscopy, each fibroid is destroyed by applying energy through a small needle array. The surrounding normal uterine tissue is not affected. The destroyed tissue may then be completely reabsorbed. It is not recommended for patients that desire pregnancy afterwards. Learn more about Acessa Radiofrequency Ablation of Uterine Fibroids
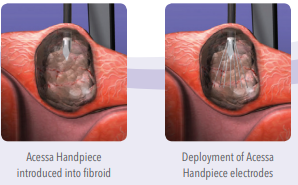
Sonata – The Sonata procedure is a new minimally-invasive, same-day (outpatient) therapy for fibroids. It uses a technology called radiofrequency ablation. It is performed through the uterine cervix accessed vaginally without incisions, with each fibroid destroyed by applying energy through a small needle array. The surrounding normal uterine tissue is not affected. The destroyed tissue may then be completely reabsorbed. It is not recommended for patients that desire pregnancy afterwards.
Learn more about Sonata transcervical fibroid ablation
Myomectomy
Myomectomy is an operation in which fibroids are removed from within the uterus. Stitches are used to bring the walls of the uterus back together. For women with symptomatic fibroids who desire future childbearing, myomectomy is the best treatment option
Myomectomy is a very effective treatment, but fibroids can re-grow. The younger a woman is and the more fibroids present at the time of myomectomy, the more likely she is to develop fibroids in the future. Women nearing menopause are the least likely to have problems from fibroids again.
A myomectomy can be performed several different ways. Depending on the size, number and location of your fibroids, you may be eligible for an abdominal myomectomy, a laparoscopic myomectomy or a hysteroscopic myomectomy.
Abdominal Myomectomy – Abdominal myomectomy, also known as an “open” myomectomy, is a major surgical procedure. Patients are asleep during the operation. An incision is made through the skin on the lower abdomen (“a bikini cut”). The fibroids are removed from the wall of the uterus. The uterine muscle is sewn back together using several layers of stitches. The typical recovery involves 2 nights in the hospital and 4-6 weeks resting at home. The procedure results in a 4-inch horizontal scar near the pubic hair or “bikini” line. Blood loss during the operation may necessitate a blood transfusion. Some women store their blood before the operation in order to receive their own blood back rather than receive blood from the blood bank. About 5% of women will develop a postoperative infection that is treated with antibiotics in the hospital for as many as 5 days. About 5% of women develop a wound infection. Although the wound infection is treated at home, women must make frequent visits to the doctor’s office for up to six weeks. After a myomectomy, the doctor may recommend a cesarean section (C-section) for the delivery of future pregnancies. This is done to reduce the chance that the uterus could open apart during labor. The need for C-section will depend on how deeply the fibroids were embedded in the wall of the uterus at the time of removal. New fibroids can develop resulting in recurrent symptoms and additional procedures.
Laparoscopic Myomectomy – Only certain fibroids can be removed by laparoscopy. If the fibroids are large, numerous or deeply embedded in the uterus, then an abdominal myomectomy may be necessary. Laparoscopy is performed in the operating room with the patient asleep. Four 1-cm incisions (cuts) are made in the lower abdomen: one at the navel (belly button), one below the “bikini” line (near the pubic hair), and one near each hip. The abdominal cavity is filled with carbon dioxide gas. A thin, lighted telescope is placed through an incision so the doctors can see the ovaries, fallopian tubes and uterus. Long instruments, inserted through the other incisions, are used to remove the fibroids. The uterine muscle is sewn back together. At the end of the procedure, the gas is released and the skin incisions are closed. Small scars remain in the skin. The typical recovery involves 1 night in the hospital and 2-4 weeks resting at home. Sometimes during the operation, it is necessary to switch from a laparoscopic myomectomy to an abdominal myomectomy. Complications from laparoscopy include injuries to internal organs and bleeding. Also, the uterus may be less strong after surgery. Therefore, women planning to become pregnant in the future, are usually encouraged to have an open, abdominal myomectomy. New fibroids can grow resulting in recurrent symptoms and additional procedures. Learn more about robotic myomecomy.
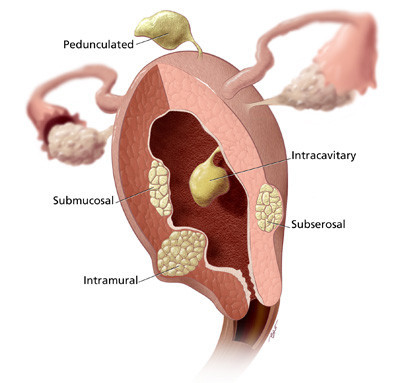
Hysteroscopic Myomectomy – Only women with submucosal fibroids are eligible for this type of myomectomy. Fibroids located within the uterine wall cannot be removed with this technique. Hysteroscopic myomectomy is an out-patient surgical procedure. Patients go home after several hours of observation in the recovery room. The operation is usually performed with patients asleep. Women lie on their backs with their feet held in gynecology stirrups. A speculum is placed in the vagina. A long, slender “telescope” is placed through the cervix into the uterine cavity. Fluid is introduced into the uterine cavity to lift apart the walls. Instruments passed through the hysteroscope are used to shave off the submucosal fibroids. There can be cramping and light bleeding after the procedure. The typical recovery involves 1 to 4 days of resting at home. There are no scars on the skin after the procedure. Learn more about Myomectomy.
Hysterectomy – Hysterectomy is a major surgical procedure in which the uterus (womb) is removed. Many women choose hysterectomy to definitively resolve their fibroid symptoms. After hysterectomy, menstrual bleeding stops, pelvic pressure is relieved, frequent urination improves and new fibroids cannot grow. A woman can no longer become pregnant after a hysterectomy. There are several different surgical approaches. A vaginal hysterectomy involves removing the uterus through an incision in the vagina. An abdominal hysterectomy is performed through an incision on the lower abdomen. A laparoscopic hysterectomy is accomplished through four tiny incisions on the abdomen. The type of hysterectomy will depend on the size of the uterus and several other factors. The ovaries are not necessarily removed during a hysterectomy. Women should discuss the pros and cons of ovarian removal with their physicians.
Vaginal Hysterectomy – A vaginal hysterectomy is performed by removing the uterus through the vagina rather than through an incision (cut) on the abdomen. To be eligible for a vaginal hysterectomy, the uterus cannot be too large. The surgery is usually performed with the patient asleep. Most women stay 2 nights in the hospital. The recovery involves significant pain for 24 hours and mild pain for 10 days. Full recovery usually takes 4 weeks. After a vaginal hysterectomy, there are no scars on the skin. Complications from the surgery include bleeding, infections and an injury to the intestines or bladder.
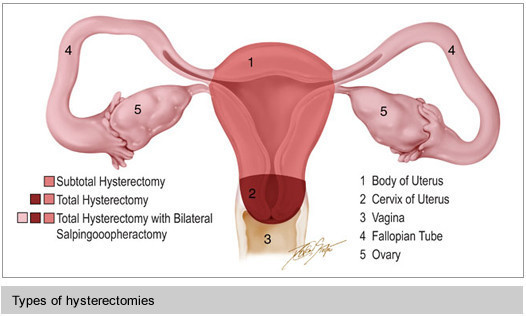
Abdominal Hysterectomy – An abdominal hysterectomy is performed by removing the uterus through a horizontal incision (cut) on the lower abdomen (“a bikini cut”). If the uterus is very large or if there is a scar from an earlier operation, it may be necessary to make a vertical incision on the lower abdomen. A total abdominal hysterectomy means removing the uterus and the cervix (the lowest part of the uterus). Women who have had abnormal pap smears or cervical dysplasia are usually encouraged to have their cervix removed at the time of hysterectomy. A subtotal or supra-cervical hysterectomy means removing only the upper part of the uterus. It is possible that women who retain their cervix will have less bladder leakage and vaginal relaxation later in life. However, it has not been scientifically proven to improve these outcomes. Women who have had a supra-cervical hysterectomy will continue to need periodic pap smears. In addition, some women will have monthly spotting or light bleeding if endometrial glands are still embedded in the cervical tissue. An abdominal hysterectomy requires general anesthesia. The usual hospital stay is 3 days. The procedure results in a 4 inch horizontal scar near the pubic hair or “bikini” line. The typical recovery involves 6 weeks resting at home. Some women experience a complication that requires a longer recovery time. About 5% of women develop a post-operative infection that is treated with antibiotics in the hospital for as many as 5 days. About 5% of women develop a wound infection that is treated at home but requires frequent visits to the doctor’s office for wound care for up to six weeks. Other complications include bleeding, infection and injury to the intestines or bladder. Learn more about hysterectomy.
Laparoscopic Hysterectomy – Laparoscopic hysterectomy is a new procedure in which the uterus is removed through very small incisions on the lower abdomen. The cervix, or lower portion of the uterus, remains in place. Women with large fibroids may not be candidates. If the uterus is large then an abdominal hysterectomy may be necessary. Laparoscopy is performed in the operating room with the patient asleep. Four 1-cm incisions (cuts) are made in the lower abdomen: one at the navel (belly button), one below the “bikini” line (near the pubic hair), and one near each hip. The abdominal cavity is filled with carbon dioxide gas. A thin, lighted telescope is placed through an incision so the doctors can see the ovaries, fallopian tubes and uterus. Long instruments, inserted through the other incisions, are used to remove the uterus. A special instrument is used to cut the uterus into smaller segments for removal through the small incisions. At the end of the procedure, the gas is released and the skin incisions are closed. Small scars remain in the skin. The typical recovery involves 1 night in the hospital and 2-4 weeks resting at home. Sometimes during the operation, it is necessary to switch from a laparoscopic hysterectomy to an abdominal hysterectomy. Complications from laparoscopy include injuries to internal organs and bleeding.
What about my ovaries? – The ovaries are not necessarily removed during a hysterectomy. The ovaries may be removed if they look abnormal or if the patient wants to decrease her chance of developing ovarian cancer later in life. In general, if a woman is in menopause or close to menopause, then the ovaries are removed at the time of the hysterectomy. Removal of the ovaries in a pre-menopausal woman can lead to hot flashes, vaginal dryness and other symptoms. Learn more about hysterectomy.
Uterine Artery Embolization (UAE)
Uterine artery embolization is a relatively new treatment alternative to open surgery for symptomatic fibroids. Embolization means blocking the blood flow to the fibroid. By stopping the blood flow, the fibroid begins to die and shrink in size. This will often decrease menstrual bleeding and symptoms of pain, pressure, urinary frequency or constipation.
The procedure is performed in the radiology department of the hospital. A doctor of Interventional Radiology will perform the procedure. The night before the treatment you should have nothing to eat or drink after midnight. You may take any medications that you usually take in the morning with a small sip of water. No aspirin, advil, motrin or ibuprofen should be taken for 5 days before the procedure. All of these medicines can thin your blood. (If you take coumadin, plavix, lovenox, glucophage or heparin, please speak to your doctor about when to stop these medicines.) See How To Prepare For Your Arteriogram for further general information. The procedure takes approximately two hours.
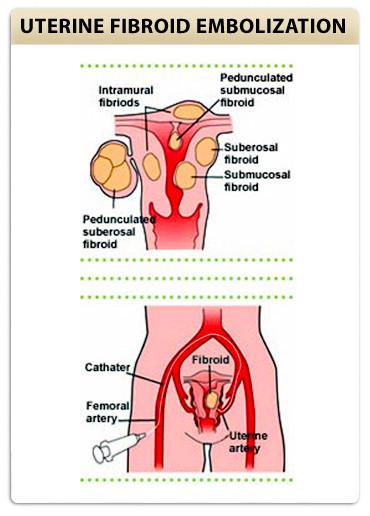
During the procedure, an intravenous line is started prior to beginning the procedure. You will then be sedated and are awake but sleepy throughout the procedure. A needle is placed in an artery in your leg, at the groin crease. A small catheter is then placed into the artery and dye is injected while x-rays are performed to get pictures of the arteries (arteriogram) that supply the uterine fibroid(s). The catheter is then used to select these arteries and particles are used to block the flow of blood. The particles are called polyvinyl alcohol and are the size of a grain of sand. These are mixed with contrast and injected slowly while we watch to assure that they go only to the fibroid. It takes several minutes to block arterial flow. After the left and right uterine arteries are embolized, a repeat arteriogram is performed to confirm the completion of the procedure. The catheter is removed and pressure is held over this area for approximately 15 minutes. After the exam you must be on bed rest for six hours lying flat with your leg straight. The amount of pain that women experience is variable. The most significant pain usually occurs immediately following the procedure and over the next 6 hours. Our patients report this pain to be similar to menstrual cramps. Some patients experience no pain. Patients usually stay overnight in the hospital, so that we can monitor the arterial access site and provide adequate pain control. Patients are discharged home the next morning. Most patients can return to full activity in a week. Learn more about UFE.
