Vulvodynia, simply put, is chronic vulvar pain without an identifiable cause. The location, constancy and severity of the pain vary among sufferers. Some women experience pain in only one area of the vulva, while others experience pain in multiple areas. The most commonly reported symptom is burning, but women’s descriptions of the pain vary. One woman reported her pain felt like “acid being poured on my skin,” while another described it as “constant knife-like pain.” Do you feel discomfort or are bothered by enlarged Labia?

There are two main subtypes of vulvodynia, which sometimes co-exist:
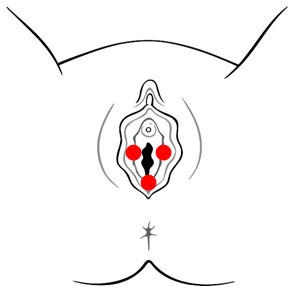
Vulvar Vestibulitis Syndrome
(aka Provoked Vestibulodynia) As shown in the diagram on the right, vulvar vestibulitis syndrome (VVS) is characterized by pain limited to the vestibule, the area surrounding the opening of the vagina. It occurs during or after pressure is applied to the vestibule, e.g., with sexual intercourse, tampon insertion, a gynecologic examination, prolonged sitting and/or wearing fitted pants.
VVS is further classified as Primary or Secondary. Women with Primary VVS have experienced vestibular pain since the first attempt at vaginal penetration. Women with Secondary VVS have experienced pain-free sexual intercourse prior to the development of pain.
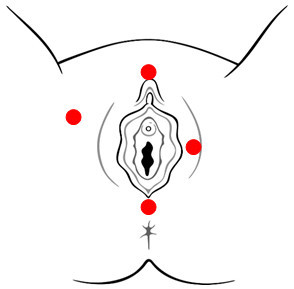
Generalized Vulvodynia
For women with generalized vulvodynia (GV), pain occurs spontaneously and is relatively constant, but there can be some periods of symptom relief. Activities that apply pressure to the vulva, such as prolonged sitting or simply wearing pants, typically exacerbate symptoms.
Some women experience pain in a specific area, e.g., only in the left labia or near the clitoris, while others experience pain in multiple areas, e.g., in the labia, vestibule, and clitoris. In the latter group, pain may also occur in the perineum and inner thighs, as demonstrated in the diagram on the right.
What Causes Vulvodynia?
Vulvodynia is not caused by an active infection or a sexually transmitted disease. Through continued research efforts, we move closer to uncovering the underlying cause(s) of vulvodynia. Researchers speculate that one or more of the following may cause, or contribute to, vulvodynia:
- An injury to, or irritation of, the nerves that transmit pain and other sensations from the vulva
- An increase in nerve fiber density in the vulvar vestibule
- Elevated levels of inflammatory substances in the vulvar tissue
- An abnormal response of different types of vulvar cells to environmental factors such as infection or trauma
- Altered hormone receptor expression in the vulvar tissue
- Genetic susceptibility to chronic vestibular inflammation
- Genetic susceptibility to chronic widespread pain
- Genetic factors associated with an inability to combat vulvovaginal infection
- A localized hypersensitivity to Candida (yeast) or other vulvovaginal organisms
- Pelvic floor muscle weakness or spasm
Medical Management
Since vulvodynia is not simply a gynecological condition, many experts favor a multi-disciplinary approach to its management. Treatment may involve visiting a gynecologist or vulvovaginal specialist, dermatologist, neurologist, pain management specialist, urogynecologist, and/or physical therapist. Also, because vulvodynia typically affects a woman’s sexual relationships and emotional well-being, your provider may recommend a psychologist or couples/sex therapist.
Because we don’t know what causes vulvodynia, treatment is directed towards alleviating symptoms and usually provides partial or complete pain relief. Some women experience relief with a particular treatment, while others do not respond or experience unacceptable side effects. No single treatment is appropriate for all women with vulvodynia and it may take time to find a treatment, or combination of treatments, that alleviates your pain.
Current treatments include:
Discontinuation of Irritants
Health care professionals recommend eliminating over-the-counter feminine products such as perfumed bubble baths, soaps, sprays and douches that can irritate vulvar tissue. Eliminating irritants is typically the first step in treatment.
Oral “Pain-Blocking” Medications
Medications that are effective in alleviating other chronic pain conditions are often used in the treatment of vulvodynia. They include:
Tricyclic Antidepressants (TCAs)
Although TCAs were developed to treat depression, many controlled studies have demonstrated their effectiveness in treating chronic pain conditions. For women with vulvodynia (or other chronic pain), the dosage is usually much lower than that used for the treatment of depression. To minimize side effects, it is best to start at a very low dose and increase the amount gradually; consequently, it can take several weeks to achieve a therapeutic level. Common side effects, which can usually be managed, include drowsiness, dry mouth, constipation and dizziness. The severity of the side effects depends on which TCA you take, e.g., amitriptyline causes stronger side effects than nortriptyline or desipramine. If you decide to stop taking a TCA, it should be discontinued gradually.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
SNRIs, a relatively new type of antidepressant, work differently than the TCAs. These medications are FDA-approved to treat depression and anxiety disorders, as well as certain types of pain, such as fibromyalgia and peripheral neuropathy. SNRIs are also used “off-label” to treat other chronic pain disorders. The most common side effects, some of which improve over time, include headache, nausea, insomnia, sexual dysfunction, dry mouth and dizziness. It can take many weeks to months to reach a dose that will alleviate pain. If you decide to discontinue a SNRI, you have to taper it slowly. Two SNRIs, venlafaxine and duloxetine, have been used to treat vulvodynia, but their effectiveness has not been tested in large controlled studies.
Anticonvulsants
Medications developed to inhibit seizures can also be effective in controlling some chronic pain syndromes. For example, the anticonvulsant pregabalin is FDA-approved to treat postherpetic neuralgia and diabetic neuropathy. Anticonvulsants are often prescribed for women with vulvodynia, especially when pain is described as having a “shooting, stabbing or knife-like” component. The effectiveness of pregabalin, gabapentin, and oxcarbazepine in the treatment of vulvodynia has not been tested in large controlled studies. As with TCAs, it is best to start at a very low dose and increase the amount gradually. If you decide to discontinue an anticonvulsant, you have to taper it slowly.
Opioids
Pain-relieving opioids, such as oxycodone and hydrocodone, can be very helpful for short-term use during vulvodynia flares. They can also be used to relieve pain early in treatment, while you gradually increase the dosage of an antidepressant or anticonvulsant to a therapeutic level. In severe cases, when more conservative therapies fail to provide relief, long acting opioids can be used on an ongoing basis. Common side effects, which can usually be managed, include constipation, nausea and drowsiness. Opioids should not be discontinued abruptly.
Topical Medications
Topical medications applied directly to the vulva can help to alleviate pain, but some preparations contain additive substances that are irritating to the skin. Therefore, many vulvodynia experts use compounding pharmacies that make individualized topical creams and ointments without irritating additives.
Examples include:
- Topical Hormonal Creams (e.g., estrogen, testosterone)
- Topical estrogen cream can improve the health of vulvar tissue, particularly when the tissue is thin or dry because of a lack of estrogen. Recently, some experts have also emphasized the role of the hormone testosterone for women’s sexual health and recommend combining estrogen and testosterone in a topical cream.
- Topical Anesthetics (e.g., lidocaine)
- Topical anesthetic cream or ointment provides temporary pain relief and is applied directly to the vulva prior to intercourse. Typically, the numbing effect lasts 15 to 30 minutes. One study found that long-term nightly use of lidocaine resulted in sustained pain relief.
- Topical Compounded Formulations
- Medications that are normally prescribed for oral use, such as antidepressants and anticonvulsants, can also be formulated into a cream or ointment. Topical preparations either contain a single active ingredient or a combination of ingredients, e.g., an anesthetic and antidepressant. Compounded topical formulations may be used in conjunction with oral medications and other treatments.
Pelvic Floor Muscle Therapy
Courtesy of Dr. Howard Glazer Some women with vulvodynia also have pelvic floor muscle weakness or spasm. In addition to evaluating pelvic floor muscles, a physical therapist should assess joints, muscles and nerves in the lower half of the body to determine if they play a role in vulvar pain. Treatments include exercise, education, and manual therapies, such as massage, soft-tissue work and joint mobilization. Modalities such as heat/cold, ultrasound and electrical stimulation may also be helpful.
In addition, rehabilitation of the pelvic floor muscles may include insertion of a vaginal sensor and the use of a biofeedback machine (pictured on right). The machine provides visual feedback on the strength of pelvic floor muscles while performing exercises to normalize their function. This type of biofeedback is conducted by specially trained providers and some physical therapists.
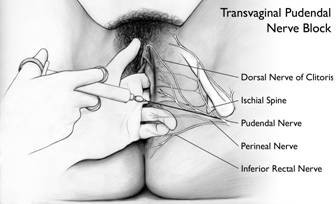
Nerve Blocks
The pudendal nerve carries pain signals from the vulva to the spinal cord. A nerve blocks for vulvodynianerve block is an injection of anesthetic, sometimes combined with anti-inflammatory medication, which ‘breaks up’ the transmission of the pain signal. In many cases, a series of injections, spaced days or weeks apart, is administered intravaginally (pictured on the right) or in the epidural space in the lower back (same as during childbirth). Most women experience short-term relief with this procedure and some experience long-term relief. One recent study found that women with vulvodynia who underwent a series of different nerve blocks (vulvar, pudendal and spinal) experienced sustained pain relief.
Diet Modification
Some women find that eating a certain food increases their pain and that elimination of the food alleviates it. For example, some eliminate acidic or high-sugar foods. If you want to test for food sensitivity, eliminate one item or food group at a time, so you can determine which ones, if any, are affecting you. With the use of a food diary, you may begin to notice an association that you wouldn’t otherwise suspect.
Neurostimulation and Spinal Infusion Pump
In severe cases, when more conservative forms of treatment haven’t worked, neurostimulation or implantation of a spinal infusion pump may be recommended. Neurostimulation involves the implantation of an electronic device that delivers low voltage electrical stimulation to the spinal cord, or a targeted peripheral nerve, with the intent of substituting a tingling sensation for pain. Spinal infusion pumps continually administer very small amounts of medication to the spinal cord and nerve roots.
Counseling
Since living with chronic vulvar pain usually affects a woman’s sexual relationship and can lead to anxiety and/or depression, some women find it helps to see a psychologist or a couples/sex therapist.
Complementary or Alternative Medicine
Women with vulvodynia, as with all forms of chronic pain, may benefit from using alternative therapies in conjunction with traditional medical treatments. There are many complementary therapies available.
Surgery (for women with Vulvar Vestibulitis Syndrome/Provoked Vestibulodynia)
Of all surgical procedures used, a vestibulectomy with vaginal advancement appears to be the most effective, with significant success rates for patients with vulvar vestibulitis syndrome. Appropriate patient selection for surgical procedures is critical to a successful outcome. Some physicians have also reported successful outcomes using a modified surgical procedure, involving the removal of small, painful areas, rather than the entire vestibule. A detailed description of how a vestibulectomy with vaginal advancement is performed, including diagrams and actual photos from surgical patients, can be viewed online.
